Guest Blog for CDN – Off to work and all of the changes that come with it: Abby’s experience
Original post here!
If you were like me, you were so prepared for the transition to college that you had checklists, extra supplies, and plans on how to engage in courageous conversations with your roommate(s). If you were like me you had researched the type of food in the dining hall and talked through a meal plan with your care team. It seemed as if I had been preparing for this college transition my whole ‘diabetic’ life. Fast forward through those four years with peaks and pits and by the time I felt I had a small grasp on diabetes management in college, it was time for graduation. So what comes next? What happens when there isn’t the same structure or checklist for the next transition?
Change in physical environment
One thing to expect for the transition OUT of college is a change in your physical environment. IN college I physically lived on campus, with roommates and I felt I was always surrounded by classmates, colleagues, and friends. So when I lived alone, not only was I processing new feelings of loneliness as a product of my new living situation, but my built-in safety net of oversight was gone. All that means is that you have to take extra precautions to prevent emergencies, even more than you did in college. One app that I have found particularly helpful is Sugarmate. One of the features is that during a set time period, you will receive a phone call if you reach a certain level. For me (a heavy sleeper who doesn’t wake up to my Dexcom alarms) that is 65mg/dL between 1 am and 6 am. It has been super helpful in catching those pesky and dangerous overnight lows.
Unlike in college, those around you may not see you managing your diabetes in the ways they did in the college environment. This means, utilizing courage, if needed, to vocalize when I may need help. For example, if I catch a low or I am sick with a high that may need advanced treatment, I may send a premature text to a trusted friend saying, “Hey, I am treating an extremely low blood sugar right now”, send them my location for an hour and then say “if I don’t text you back in 15 minutes call me. If I don’t answer three times call an ambulance to my location.” Yes it seems intense and usually I am fine and text back the minute I start feeling better, but I would be remiss if I didn’t prepare for the “what ifs”.

Change in mental space
Similarly to the transition TO college, the transition FROM college includes a change in mental space and I realized I needed to adjust my mindset, particularly with harnessing more personal accountability. Gone are the days of “oh I am in college and my schedule is crazy” and giving myself a “pass” on holding myself accountable for what I was eating, drinking, how much I was working out and sleeping. Post-college I found a daunting, yet exciting opportunity to face these challenges head-on. I chose a career with more routine hours, that left me time to cook, and if I wasn’t sleeping it was not because I had too much homework or a late shift at work, it was because I made the choice to stay up late and therefore had to face the consequences. There were a lot of behaviors to unlearn, which isn’t unlike other young adult’s transition out of college, but I also had to learn patience and grace because the path to success wasn’t linear. Transitioning from college meant facing the real reasons why I may have had poor management including a lack of focus on eating and exercise, laziness when it comes to looking up carb counts, and a general lack of self-discipline. All of that can feel like a whole new level of burden. That means digging into the “coping mechanism toolbox” that we have all been forced to learn from a young age to maintain a healthy perspective about living with a chronic illness.
Change in emotions
With the change in mentality around diabetes management, I think my emotions changed too. I was very lucky to be plugged into CDN at an early stage in college. Talking about diabetes with others arose naturally when I other people with diabetes. Even if it was just a sentence acknowledging a triumph or a challenge from that week, sharing that with someone who understood was very therapeutic. I didn’t realize what the power of vocalizing something seemingly routine, had on staving off feelings of isolation that we all know too well. I realized that I have fewer people who “get it” outside of the CDN community on campus. So what do you do? I started talking more openly with my friends, and they have been receptive. You just have to do it. I find the more I talk to them about it, the more questions they ask and the more I educate them on it, and soon they start to understand enough where they can be genuinely supportive. I always felt like I would annoy people with my diabetes but people are actually really willing to learn and listen to what one of their friends goes through on a day-to-day basis. It was scary at first, but now I am maintaining a level of emotional support that I didn’t know I needed until it was gone.
Just like transitioning INTO college was a huge, scary, intimidating transition, transitioning out of college will be too. But, in a weirdly beautiful way, managing your diabetes can be the thing that grounds you; the normalcy in a changing world. You still have to count carbs, administer insulin and respond to low and high blood sugars, just like you did before college, just like you did while in college and just like you will continue to do.
AB
When it’s my turn to be the Cheerleader.
And why it’s long overdue.
A lot of people throughout my life have told me that I am so strong, an inspiration even. I don’t always understand this because I am just living my life like anyone else.
What I do know for certain is that behind me, is a strong mother cheering me on, constantly learning how to best support me, who taught me how to get back up and not depend on anyone.
When you see the smiles or the jokes about diabetes, it is because my mom has handled the hours of defeat, sadness, frustration and disappointment because of this disease. She is the “punching bag” for diabetes, even though she does not deserve that role. She takes it on, so no one else has to.
When you see me being able to walk and bike and advocate, it is because without anyone asking her to, my mom became deeply committed to doing EVERYTHING to making my life and my family’s life better. She will drop everything, take time off work and re-prioritize so that I can follow my dreams and advocate/lobby for a better future.
When you see me beaming with pride with the newest technology it is because my mom has researched and researched and had countless conversations about what would be best for me. It’s because she has fought insurance companies and become an expert on things, no mom should have to.
When I get acknowledged for my independence it is because of my mom, because she instilled that mindset early. Its because she let me try my first fingerstick by myself, as a five-year-old, just a day after being told my life would never be the same. Its because she let me take over most of my management at a young age and its because she bit her tongue, let me take risks and helped me ride out the consequences when I bit off more than I can chew.
When you see me just living my life, its because that mindset came from my mom. She always said from a young age that I would do everything we would do before diabetes, with just a few extra tasks each day. She did that. She took a life-changing diagnosis and boiled it down to bite-size two and three-minute adjustments, to make it tangible for my five-year-old self and my family. My mom had the forethought and the focus after an overwhelming day to create that mindset.
I mean just two days after being diagnosed with diabetes, she’s dealing with new routines, educating family, thinking about my life at school so I could be focused on what was still most important to me at that time, learning to ride my bike without training wheels. She took on the burdens, and continue to take on the burdens in discreet and indirect ways, so I could dance, play sports, go over to sleepovers, learn to drive, go to college and be my quirky, outspoken self, without losing my spark.
You have to truly be selfless to be a caregiver for this disease. I don’t just have diabetes, she has it too, my whole family does. She may not feel the physical pain of needles piercing the skin, the heavy sleepiness, dry mouth and moodiness that comes with high blood sugar but she can see the life and energy leave my body by just looking at me. My mom (and dad) can look at me and just tell if my blood sugar is low, just by looking at my zoned out eyes and pale skin. It is actually quite remarkable.
My mom has truly dedicated herself to this cause, to me, to my family, to those we have lost. And I don’t thank her or acknowledge her enough.
So now its my turn. To cheer her on and lift her up and she gets ready for the #JDRF Saratoga Springs ride and is riding over 100 miles to raise money for diabetes research! SHE is the epitome of strength. SHE is the epitome of turning setbacks, fears and frustration into motivation. SHE has never and will never stop believing. Give this a like and go share a good luck post on her wall if you can!
It’s not even too late to donate! https://www2.jdrf.org/site/TR…
#ridetocurediabetes #typeonetotypenone #jdrf #t1d
AB
I am more than a number.
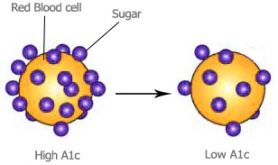
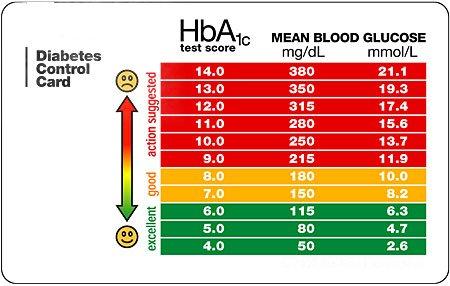
People with diabetes live by numbers. But there is no number more highly regarded, than the A1C number. Measured through a blood test, hemoglobin A1C, provides information about average blood sugar levels over the past three months.
When I go to my endo appointments every 3 months, the only thing my mind is focused on is getting my A1C results. That’s it. I am thankful to have technology today that allows for almost immediate results because back in the day I would have to check our mailbox every day the following week, for that letter with the highly anticipated results.
Usually it is about two or three days before my appointment that I realize I even have an appointment. It is at this time that my stomach drops, my heart starts pounding a little faster and my brain starts to go over every time I forgot a bolus, or let a high blood sugar linger for just a little too long. What ensues is two or three days of diligence, and perfect diabetes management. Unfortunately I, like many others, have learned the hard way that you cannot improve three months of lack-luster management in three days; even though we incessantly try every time.
That 2 digit, sometimes 3 digit (throwback to sophomore year of college) number, is so important to people with diabetes. In addition to being the only thing we think about leading up to an appointment, it can also set the tone for the entire appointment, which is actually quite counter productive. It doesn’t stop there. A1C will continue to float around in our heads for the rest of the day or more, after the appointment. I love seeing diabuddies triumphantly post the results of an improved A1C on social media as much as the next person, but I also know what those long car rides home feel like after not receiving the results you (unrealistically) hoped for. It’s usually the first thing my family members or even other diabetics are itching to know, whether they verbalize it or not.
I mean think about it, even when you go to the eye doctor or primary care doctor, it’s the first thing they ask. If it is higher than a 6.0, I feel the need to quickly justify it, with, “Oh, but I’m very active.” or “Oh, but it’s lower than last time” as I try to avoid their judgmental gaze or tone in their voice. But it is not their fault, A1C is the only way that these healthcare professionals have been trained on how to assess someone’s blood glucose control.
It is like having tunnel vision for this number. But why? Why do we focus on it so much? Why do I absorb nothing else from the appointment, besides that number? It’s because we have been taught that the A1C is a grade. We’ve been taught that A1C is a permanent part of our diabetic identity. We think of it as not only a judgement of our diabetes management for the past three months, but also a judgement of ourselves. We, as people with diabetes, take this number very personal.
Whether intentional or not, I have been conditioned to think that an A1C in the 6’s is an A+ and anything above 7.5 is failing. If that was the case, I would have failed out of “controlling my diabetes” when my A1C was 10.2 during my sophomore year of college. The amount of stigma and guilt there is around a high A1C is very burdensome and leaves the person with diabetes feeling helpless, rather than motivated to make necessary adjustments.
But the thing is, I didn’t need an A1C to tell me that I had poor diabetes management. I looked at other factors to gauge how well I was doing. I was tired all the time, sleeping in class, sick a lot, I was not testing my blood sugar, my time in range was minimal and overall I just felt burnt out. The A1C was a reflection of all of this; “all of this” was not a reflection of the A1C.
Even the way we market or educate ourselves on A1C can have alternate meanings. A1C is just a snapshot, not the full picture.
I think that it is important to acknowledge that A1C carries a lot of weight in looking at glucose control, but it doesn’t hold all of it. Because it can be very misleading, and it is necessary to look at other factors and other outcomes. A lower or “good” A1C may actually indicate severe low blood sugars over night. Sometimes a higher or “bad” A1C means you are mostly in control, except for post meal spikes. Or it could even mean that you’re on the swim team and you practice twice a day with your pump off so naturally, you are constantly trying to catch up on your basal. Even if you are diligent, there just may not be a lot of pay off. We so strongly correlate low A1Cs with the amount of effort a person with diabetes is putting forth forgetting the fact that A1C is not, and should not be, the only outcome measure for diabetes management.
I mean even in schools we tend to follow a similar philosophy. It’s about being well-rounded. My parents excused C’s because I was also on the field hockey team, in band, a leader in the student council and on the science Olympiad team. Or if they knew I was trying hard, I was not shamed for the grade I received. We looked at other outcomes, to base action off of, to help improve my academics. There was so much more to high school than just my grades, just like there is so much more to diabetes than a number.
Luckily with the support of my mom and my diabetes care team I have broken this cycle of toxic thoughts around A1C. And thank goodness for that. We focused on specific times I was not in range. We focused on my activity level, my food intake, overnight trends, and most importantly how was I feeling? Was I balancing being a normal young adult with focus on diabetes management? We looked at the smaller adjustments to be made, that would have an impact on bringing my A1C down to where it needed to be. Having good control doesn’t necessarily mean a good A1C, but also good mental health, physically feeling well and not being bogged down by every aspect of diabetes.
It is no doubt that A1C is the most known way to judge the control of your diabetes. And even though it is one small part of the entire management picture, the reality is, is that currently A1C is the only UNBIASED way to measure diabetes management. It’s the only quality measure used to approve diabetes drug therapies. But it’s time to change that.
Next week there is a FDA workshop between patient groups, industry and the Center for Drug Evaluation and Research (CDER) on Outcome measures beyond A1C. I have been lucky to be able to help market and prepare for this event through my Students with Diabetes internship this summer. And we need you to be involved too!
First, help us share the patient perspective with the FDA. Create a short video. Here’s an example. This is a unique opportunity to bring YOUR voice directly to a FDA meeting.
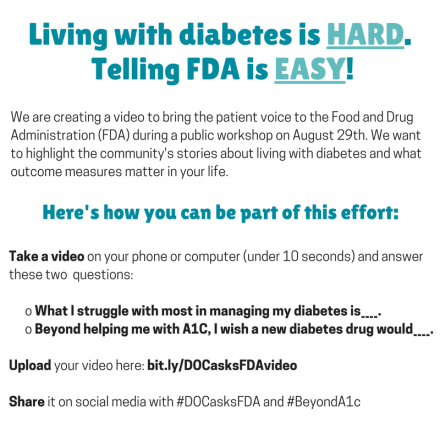
Submit videos here.
Then, register to attend the event in person, or via webcast, here.

Also check out what people are saying in the diabetes blog-sphere (post from Diabetes Mine), this one (from It’s all about Balance) and this one from Manny at Tudiabetes.
And lastly, spread the word on social media with the hastags #DOCasksFDA and #beyondA1c
We are more than a number. We are more than our diabetes. And it’s about more than A1C.
AB
Intern Spotlight.
My summer internship experience would not have been even half as good if it were not for all of the great staff at HCM Strategists. Especially the fellow intern on the health team, Stephen Gamboa.

Some things you should know about Stephen is that he is a few years older than me, has a master’s degree and just completed a distinguished fellowship at AIDS United. He is on his way to grace Columbia Law school with his intelligence, drive, and strong work ethic. He’s so hard-working that he would G-chat me about projects on Friday’s, even though it was his day off.
Like me, he has a passion for health policy, advocacy, and making a difference in patient’s lives. He is wicked good at answering and transferring the phones, knows a lot of about hospital systems and was eager to learn more about diabetes and the Dexcom CGM system.
Stephen was great to rehash the weekend with on Mondays, was always down for Chipotle, and even though he may have won (by a slim margin) in our Meeting Schedule Competition, I knew we would get along when he shared his favorite Mean Girls movie quote, and that he also prefers to eat ramen without the broth.


Here’s a spotlight on Stephen, hope you enjoy.
AL: Where are you from originally?
SG: I am originally from Albuquerque, New Mexico.
AL: Where did you complete your undergrad?
SG: I completed my undergrad and a master’s degree at Arizona State University in Tempe, Arizona
AL: What are your degrees in?
SG: For undergrad – I majored in Music Performance and was also Pre-Med. My Master’s degree is a Master of Healthcare Innovation
AL: What other internships and fellowships have you held? What are most memorable moments or times from those experiences?
SG: 1) Mayo Clinic Premedical Scholar – I really enjoyed shadowing doctors and nurses and getting a feel for the clinical side of healthcare. This was especially inspiring to me at the time because I was interested in a career in medicine.
2) Southwest Center for HIV/AIDS – I interned here for a year during my Master’s degree and I helped manage a research program called Integrated Collaborative Care. This program served as a holistic model of healthcare delivery for 75 research participants and I helped both with the logistics as well as some of the data analysis. This was an amazing opportunity to see how research can have a real impact on the daily lives of patients.
3) AIDS United Pedro Zamora Public Policy Fellow – This was my first job out of school and my favorite memory was going to the annual Presidential Advisory Council and on HIV/AIDS meeting. During this meeting, I got to see a lot of leaders in the field come together and talk about issues and suggest solutions for the federal government to pursue.
AL: What do you do in your spare time?
SG: I’m a big runner and am currently training for the Marine Corps Marathon so I spend a lot of time outside of work either running, at the gym, or in a spin or yoga class. Additionally, I love checking out new places in Washington, DC since I’ve only been here for a year and eating really good food!
AL: What’s your favorite food?
SG: I love French cuisine, so Le Diplomat on 14th St. is one of my favorite DC restaurants.
AL: Favorite spot in DC?
SG: I have two – The Hirschhorn Museum on the National Mall is great. They have really incredible exhibits and they have a great reading spot that overlooks the mall that I often find myself at. My other favorite DC spot is Rock Creek Park – I run quite a bit in Rock Creek and it’s a great way to enjoy some greenery and at least have the illusion like you’re getting out of the city.
AL: What do you think you’ve learned most from this internship experience?
SG: I’ve learned a lot about the approach to developing a public policy strategy. For example, I got to sit in on the initial planning meetings for the ISTH project and it was great to observe how HCM creates a strategy to take the organization from where they are to where they want to be. That’s a transferable skill that I think will really help me in the future.
AL: What has been your favorite part of this internship?
SG: Aside from learning a lot about building strong client relationships and creating strategy to help organizations with their public policy agendas, I really enjoyed the people. It was a great, collaborative work environment and I was able to get along well with everyone on the health team!
AL: What is next? And how do you feel about that?
SG: I will be moving to New York City at the end of the summer to pursue an MPH/JD dual degree program at Columbia University. I am very excited for this next chapter, but honestly, also just a bit nervous. We will see how it goes!
Stephen had one final DC hurrah this past week when we ventured up to the top of the Washington Monument to capture these stunning views. (pictured above)
Thank you Stephen for sharing all the advice you have on Grad School and beyond. And if we ever find ourselves meeting again, please hire me.
XX, AB
In’s and Out’s
Happy August first!
Even though we only have one month left of summer vacation, I thought I would give you guys a little insight into the in’s and out’s of my experience in DC for the summer. Off the bat I can tell you it is fun, hot, adventurous and relaxing. Oh, and did I mention hot?
I am subletting an apartment from my best friend Acadia in a building just off of American University’s campus. There I live with four other roommates, George, Kay, Kim and Sam in a two bedroom apartment. Because we all work, intern or both, it is a rare but fun occurrence when we are all home at the same time. They are really cool, nice and fun people with interests in journalism, the environment, cooking, music, film making and government conspiracy theories among others.
Everyday I get on the bus at a stop right outside my apartment building. I use a bus tracker app and I have timed it out so if I leave when the app says the bus is four minutes away, walk briskly, I make it just on time. The bus is usually packed with summer interns and professionals all making their way downtown in the muggy morning weather. I take the N4 down Mass ave onto Connecticut Ave. My friend Adrian and I both have to be at work at 9am sharp so we take the bus together most days, unless one of us is running late (cough cough Adrian ;)). Being surrounded by ambitious peers dedicating their summers to interning gets me through my mornings. Once I hit M St and Connecticut I exit the bus, yelling a “thank you” to the driver, rushing to cross the street before the next green light and walk three short blocks with a wave of fellow commuters. One really cool building I pass every day is the National Geographic Museum and I told myself that before the summer is up, I will have to go and check it out.
The 20 – 40 minute commute (depending on traffic) to and from work has really given me a chance to read. A lot. So far I have read, Save Market Basket, When Women Win, The Kite Runner, The Old Man and the Sea by Ernest Hemingway, I tried to get through 1984 but had to put it down, My Beloved World by Sonia Sotomayor. Currently I am switching between Hillary Clinton’s book, Hard Choices and Anderson Cooper’s Dispatches to the Edge. I am open to any recommendations.
For lunch, I pack it basically everyday. Both to save money and to optimize time at my desk, especially when I have many assignments to work on. Typically my lunch consists of a sandwich (I love sandwiches), vegetables (carrots, celery and broccoli), an apple or grapes, cheezits or unsalted potato crisps (my favorite) and 1 or 2 hershey’s kisses or york patty (yes, diabetics can eat sugar). One time, the other intern and I treated ourselves to Chipotle. It is just over on the next block. The fact Chipotle is so close, is dangerous because it is so good.
Living in DC is expensive so this summer I have stayed on as a part time employee at the gym on campus. I typically work a closing shift (6pm to 9:15pm) a few days a week. On those days I pack a dinner as well as lunch and bring my work t-shirt with me and go straight from the office to the fitness center. These days can be somewhat exhausting but I really enjoy my coworkers. At the gym I swipe members’ ID cards, rent out equipment and make sure any administrative paperwork is complete.

#AUrecfitfam
Then when I go home, I wait for my roommates to return, hang out with them for a bit, go through my nightly routine (make lunch, lay out clothes, ect) and do it all again the next day. Then when the weekend hits, I try new restaurants with friends who have also stayed in DC this summer, go to the pool, catch up on Netflix and take long bike rides through DC. The weekend also means doing a whole host of “adult” things like laundry, grocery shopping, cooking and cleaning.
That’s all for now. Thank you to everyone who has made this summer in DC both possible and enjoyable.
AB
I’m a diabetic girl in a diabetic world.
If you’re like me then you have type 1 diabetes and are unapologetically passionate about advocating for a cure and working tirelessly to improve quality of life for those living with diabetes. If you’re like me then you realized your career path was one in a diabetes related field. If you’re like me then one of the biggest concerns you had once deciding to pursue an opportunity in a diabetes related field, was, how would it be working on diabetes issues daily, while having diabetes? Would you be too close to the issue? Would it be difficult to separate personal experiences from work assignments? Would I become burned out?
Here are my thoughts on what I’ve learned so far since getting my internship through Students with Diabetes.
First, this is where your passion lies. Never second guess yourself on that fact. Rather, focus your efforts on how to grow professionally and learn as much as you can both on this specific topic, but also other topics -develop your skill set. At my internship I am given many of the “diabetes” assignments. But I am also asked to work on projects for non-diabetes related clients. I welcome those opportunities with open arms. The advocacy, digital, research and communication skills that I have learned on diabetes-related work, are transferable to many other areas within the field of health. The more diverse skill-set you possess, the more future opportunities you are creating for yourself.
Secondly, it is important to separate yourself from your work. Yes, we may fall into the population that you are doing work and advocating for, but your lived experiences are not the same experiences as everyone in the diabetes community. Learn from your community, be a good listener, ask questions. The course of our disease and our treatment plans are as varied as snowflakes. Sometimes I even forget that I have diabetes and choose to work on my assignments as if I am new to the topic. There is always more to learn about your disease. When you separate yourself from your disease, you will be surprised at what you will realize you did not know about diabetes. Become a student of the disease.
Thirdly, with that said, you have been given a unique opportunity to use your own lived experience to provide knowledge and insights on what living with diabetes is like. Beyond the text book definitions. You’re a patient, with a perspective, so when working with the patient perspective and voice, draw from your knowledge. Similarly you have access to connections in the diabetes community, just by living the life you have be given. You have a gift to use your diabetes to effect positive change, use it.
Fourthly, I think it is especially important to take care of your diabetes. Sometimes I am so involved in my work I put my own diabetes tasks on hold. Keep yourself healthy. Otherwise you won’t be able to succeed professionally, let alone offer productive information to your work on diabetes. Have an outlet for your own frustrations with diabetes to prevent that from bubbling over into your work. The whole reason you have found yourself at a job in a diabetes related field is because of your ability to have a positive outlook on your life with diabetes. But of course it is not sunshine and rainbows all the time, the key is to not let that overcome you and resent your job.
Similarly, much of the research I have done has only further illuminated the hardships of diabetes and made me learn about issues I may not have realized existed. Some of the hardships do not impact my life at all. It is easy to get angry and fired up over those injustices and complications of diabetes. But instead of letting anger take over, channel that fire within you to create more positive change, and be the best intern or professional you can.
Lastly, Diabetes is a complex disease. Everyone with diabetes is different. Your experience is only one experience of many. The complexity of this disease is the reason you even have a job in the diabetes related field in the first place. If there was a one-size-fix-all for everyone with diabetes, and their voices did not matter, and everything was fine, there would be no need for you to pursue a career in a diabetes related field. It is important to remember sensitivity when working on these issues within this community.
This gift has allowed me to turn my setback into an opportunity. A gift to turn this chronic illness into a chronic passion. This gift has allowed me to use leadership, public speaking, and research skills to help advocate for people with diabetes. I have been given a gift of a positive attitude. I have been given the gift of someone believing in me. I have been given the gift of believing a cure will come, and I can be apart of making that a reality. I am just a diabetic girl in a diabetic world.

In range blood sugar while advocating for Medicare CGM coverage to congress.
AB
#diabetesaccessmatters.
Today was the launch of the Diabetes Access Matters campaign on the Diabetes Patient Advocacy Coalition’s (DPAC) website.
I am so excited to see the diabetes patient community unite to raise their voices against insurance companies deciding treatment plans; something that should be between patients and their doctors.
Some of the actions patients can take include:
- Sending a message directly to health insurance companies about how restricting access is harmful for patients,
- Share images along with #diabetesaccessmatters on all social media outlets,
- Send a letter to the editor of a local news outlet,
- Tweet to the top health insurance executives,
- Tweet out information out to your followers with #diabetesaccessmatters
- Share personal stories about restricted access and,
- Share the fact sheet. The more people educated about this issue, the stronger our voice becomes.
It was rewarding to have a hand in this project and can’t wait to see what change is made when the movers and shakers of the Diabetes Online Community come together.
This is the kind of stuff that gets me up in the morning. Because the thing is, this is not just an issue between one insurance provider and one manufacturer. The scope is bigger than that, and many patients are impacted by the decisions of their insurance companies.
Insurance companies have waged a war on the wrong community, and we won’t stop until every diabetic has the choice of what treatments options work best for them, and the access for them to have what they need.



Check out the press release here.
AB
If My Diabetes were a person, it could Drive.
This past week I celebrated a milestone. I celebrated 16 happy and healthy years with type 1. I gathered a group of roommates, friends, and fellow diabetics for wine and Klondike bars because… how else would you celebrate the absence of beta cells?
Everyone who experiences a day like that, vividly remembers it. It is kind of like a second birthday. Because my life “restarted” the morning of June 23rd 2000. Here is how it happened.
Our journey actually began on June 22nd at the Kindergarten physicals. After somehow collecting urine samples of two nervously rambunctious five year olds, a task within itself, mine returned with testing positive for glucose. Maybe it was a glitch at the lab? Only I got the extra “special” blood draw, not my twin brother. And that seemed to put concerns to rest when it came back normal, a little higher, but normal. Nothing to be too alarmed with yet, I was young and asymptotic, but something to keep an eye on.
But someone knew. My mom. She new. At the site of a blood sugar out of the normal 70-90 range her stomach dropped like a rollercoaster. She knew. She knew all of our lives were about to change but did not want to believe it. My mom was all too familiar with what was happening because her own brother fell victim to this disease as well. But she remained anxious, silent and in denial and experienced the next 24 hours in utter shock.
They sent us home with caricatured band aids for our booster shots and stickers. And an assignment. Tomorrow, June 23 2000, we were to report back first thing in the morning for a fasting blood sugar. Seemed fair enough to me. I got up the next morning and reluctantly skipped my usual bowl of honey nut cheerios. The seriousness in my parent’s voice indicated that I should not yet question why we were skipping our morning routine. I told myself I wasn’t hungry anyways, hoping my bravery may help relieve the worry lines that had formed on their sleepless faces.
We got there and yet another blood draw confirmed a normal fasting blood sugar. Those results lifted even more weight off my parents’ shoulders, but only for a bit. Little did we know we wouldn’t be home for family dinner that night.
After that, we were tasked with our next assignment. We were to go to the local Denny’s and get an all you can eat breakfast. Wow, June 23rd was turning into one of the best days ever. I’m talking eggs, bacon, sausage, toast with jelly, and pancakes with REAL maple syrup. I had no idea that this was the last time I would ever consume the sweetness of real maple syrup. Despite being full, I cooperatively obeyed when my parents told me to finish my plate.
Boy, was I really putting my pancreas to the test today.
I was confused as to why the pediatrician needed us back in the Dalmatian covered room, but again, I knew today was not the day to ask questions. Why did I have to have my blood drawn AGAIN? I was only two needles into my diagnosis and already unhappy with the direction this was going. Little did I know the amount of only blood tests, would reach more than 46,728 by the time I wrote this blog post—and yes, sometimes I still question why I have to do finger pricks to test my blood sugar.
Waiting for those lab results felt like an eternity. That needle in my arm was it. This was going to decide the rest of my life.
With results showing a blood sugar over 300 we were off to the hospital so fast I didn’t even notice the tears in my mom’s eyes and the change in my dad’s voice. Christopher was off to the babysitter, my mom called out of work and we were headed to the diabetes center at Upstate Hospital in Syracuse, NY. Luckily I would not need to be admitted because I was not in ketoacidosis, something that many newly diagnosed patients experience.
Before going in, my mom had to do one of the hardest things a mother could do. She was going to be the one to break the news to her five year old. She was the one who sat me down outside of the doctor’s office, looked me dead in the eyes and told me point blank that I had Type 1 Diabetes, and I would have it for the rest of my life. She slowly and carefully explained the new lifestyle we would have to adapt to. My first response was not tears, not pity, not resistance but,
“Mommy, will I go blind and never be able to see you Christopher and Daddy again?” Will I go blind. That was my first response. I was worried that I would never be able to physically see my family again. (I wish I could say that is no longer a fear of mine, but unfortunately that is an all too common complication.)
That’s the funny thing about five year olds. The only interaction I had with diabetes was with my uncle, I’d only met a few times, and some how I already understood the all too devastating impacts this life-threatening disease can have.
After swallowing the lump in her throat and fighting to hide the tears welling in her eyes, she said, “We are going to do everything in our power to make sure that never happens to you.” My mom has never forgotten our conversation on that bench.
We entered that hospital with the morning sun low in the sky and didn’t leave until after the moon had come out. Most of the day was a blur, parents talking with all different doctors, social worker reading me books about diabetes in school that I could care less about and staff giving me that wide-eyed nervous-smile look, questioning in their hearts why good things have to happen to innocent, happy, and healthy children like myself. They had seen the far too destructive reality of this disease in their career.
Of the many things that stand out that day I distinctly remember an emergency helicopter landing on the roof of the hospital. And while the patient was in critical condition and the circumstances for my own fascination were at this patient’s expense, it was a highlight of that day. It was that distinct memory that really put life into perspective. Yes, the news of diabetes was devastating and our lives were changing, but I would be able to sleep in my bed that night. At home. With my own family.
Then I remember the sprint. I swear I have never run that fast before in my life. Before my nurse practitioner could even finish uttering the word “shot” I was off my mom’s lap, out the door, down the hall, through the nurse’s station and into the playroom. Behind me was my dad, my mom carrying Pink Bunny, (pshh like a stuffed animal was going to console me in this one waiver from my brave façade that day) my life as I knew it was over. And behind them, my nurse practitioner, Kathy Bratt, with an insulin syringe in her hands.
I like to think I put up a good fight and fast run but I was no match. I was quickly held down by my dad, and punctured with the insulin syringe. After all I did just eat the real maple syrup and my body was slowly shutting down because of my broken pancreas. I think I can only sum this experience up with the word traumatic. Traumatic for all involved.
As we were pulling out of the parking lot after that exhausting and surreal day, I asked if I was going to be okay. I was just trying to gently validate and reassure that I didn’t need to be scared, once again trying to maintain the bravery I had for the past 24+ hours. She confidently responded with, “You are going to be fine, we are just going to need to do a few extra things everyday to keep you healthy.” In a very matter of fact manner, I said, “ok Mommy!”. And that’s all she needed to hear. What we all needed to hear. We are going to be fine, we just need to do a few extra things everyday.
This trauma, but also bravery, is something that all people with diabetes and their families face. Everyone’s experience is different, but it is the uniting force for this community. After all, the reason we walk, fundraiser, research and advocate is not for us, the people who have already lived this trauma. But its to prevent other families from experiencing the life changing trauma that we did on June 23 2000.
Eight hours after that breakfast on what I thought would be the best day of my life, I consumed my first dinner as a diabetic which took place with my mom and dad in the hospital cafeteria.
The day after I was diagnosed, I learned to ride a two-wheel bike. Yes, I had just been diagnosed with a life changing chronic illness and I was focused on riding without training wheels.
Two days later I actually did my own finger prick. A big enough milestone to bring a tear to my proud parents’ eyes.
A year after that I started on the insulin pump, the youngest pumper in the diabetes center.
I continued to participate in my dance recitals and soccer games with juice boxes on the sideline and my mom to reconnect me to my pump after my performances.
Three years since my last carefree meal, I experienced the magic of diabetes summer camps.
Every year after 2000, I’ve had close relationships with all the school nurses all the way up through high school.
My first meal as a diabetic in the hospital cafeteria has transformed into “special” lunches at McDonald’s or The Cheesecake Factory with my mom, dad, or best friend after my endocrinology appointments every three months.
Skip ahead to twelve years after that day being held down in the play room, I met with congress to explain why more funding for diabetes research is necessary and to push guidance on what would become the artificial pancreas.
Five years after feeling so alone, I would be at a family gathering in the same company of two of my uncles, also type 1.
Eleven years after learning on what would become out-of-date technology, I started on the revolutionary, continuous blood glucose monitor. (Then proceeded to lose it, find it and lose it again in a never ending cycle)
Thirteen years after stabbing oranges with water-filled insulin syringes I went off to college, found an extremely amazing roommate, friends and established a College Diabetes Network chapter, while discovering my passion for public policy… specifically in the field of health.
Sixteen years after making those phone calls to family members and friends, letting them know their granddaughter, niece and sister, would be living with an auto-immune disease for the rest of her life, I sit, with friends, eating Klondike bars and drinking wine reflecting on this journey.
“Abigail, Everyday we just need to do a few extra things to keep you healthy.”

AB
This ones for you.
My mom sometimes has a lot of feelings about diabetes. I have created a space just for her! Sometimes the person with diabetes and the parent can view the same situation very differently. The only way we have learned to make it work is by taking in to account both of our perspectives and logic for a certain situation.
AB and Jeanine.











